- Optum Provider Portal – www.optum.com
- Basic Information on uhc (Umc, Optum) provider portal
- UHC (UMC) Provider Portal – www.uhcprovider.com
- Phone Number for Claim Status
- How to claim through Optum Provider Portal?
- Timely Filling Limit
- Phone Number for Claim Status – UnitedHealthcare Provider Portal
- How to claim in uhc (Umc) provider portal online?
- Important Links
- Further Asked Questions
uhc (Umc, Optum) provider portal, Phone Number for Claim Status, Timely Filling Limit: Check full information on uhc (Umc, Optum) provider portal. check phone number to claim status. Also timely filling limit is also given. Follow steps given below to claim services now under Uhc Provider Portal.
Optum Provider Portal – www.optum.com
Optum Provider Portal Claims Quick Reference Guide contains all claims submission information. You can also find reconsideration process in Optum Portal. Optum provides Optum Provider Portal, a leading health services and innovation company. The portal is designed to help healthcare providers manage various aspects of their practice, including patient information, claims processing, and communication with insurance companies. Submit a claim through the Optum Provider Portal at www.optum.com and select a type of service you’re providing and the contract you have with Optum.
Basic Information on uhc (Umc, Optum) provider portal
| Title | uhc (Umc, Optum) provider portal, Phone Number for Claim Status, Timely Filling Limit |
| Portal name | UHC (UMC, Optum) Provider Portal |
| Year | 2024 |
| Category | Claim services |
| UHC Full form | UnitedHealthcare |
| Timely Filling Limit |
|
| Phone Number for Claim Status | 1-866-509-1593 |
| Mode of Claim | Online Mode |
| Official Website | www.optum.com or uhcprovider.com |
UHC (UMC) Provider Portal – www.uhcprovider.com
UHC (UMC) is one of the largest health insurance providers in the United States. UMC stands for United Medical Center, while UHC likely stands for UnitedHealthcare. UnitedHealthcare (UHC) provider portal, it an online platform designed for healthcare providers who are part of the UnitedHealthcare network.
This portal allows healthcare professionals to manage various aspects of their interactions with UnitedHealthcare, such as verifying patient eligibility, submitting claims, checking the status of claims, and accessing other resources and tools related to patient care and insurance billing.
Phone Number for Claim Status
| Address | Claim Area |
| Optum Care Claims
P.O. Box 2500 Rancho Cucamonga, CA 91729 |
Northeast Connecticut |
| Optum Care Claims P.O. Box 30788 Salt Lake City, UT 84130 |
Pacific Northwest • Oregon • Washington |
How to claim through Optum Provider Portal?
General process for submitting a claim through Optum Provider portals, follow steps given below:
- Log In: First, log in to the Optum Provider Portal using your credentials at – www.optum.com or through a registration process to obtain login credentials.
- Access Claims Section: Once logged in, navigate to the claims or billing section of the portal. This is typically where you can initiate a new claim submission.
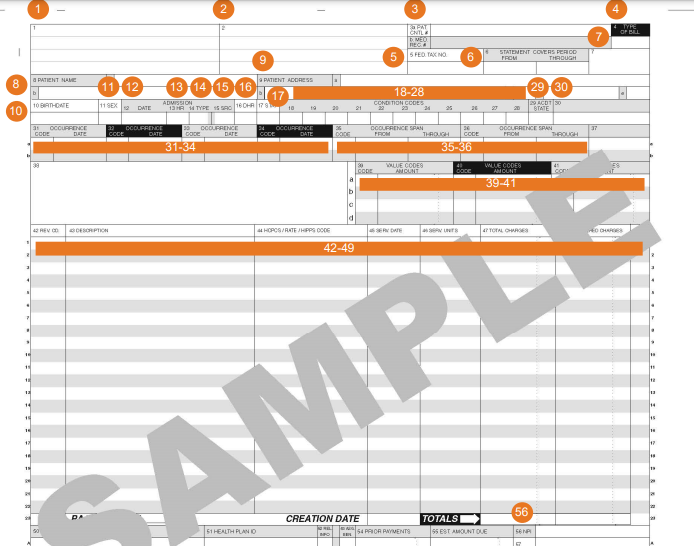
- Fill Out Claim Form: You’ll likely need to fill out an electronic claim form. This form will ask for details such as patient information, the type of service provided, diagnosis and procedure codes, dates of service, and provider information. Make sure to enter all information accurately, as errors can lead to claim denials.
- Attach Documentation: Depending on the type of service, you might need to attach supporting documents, such as invoices, medical records, or other relevant documentation to the claim form.
- Submit the Claim: After filling out the form and attaching necessary documents, there should be an option to submit the claim electronically and save the claim as a draft
- Confirmation: After submission, you should receive a confirmation message on your registered mobile number and indicating that your claim has been successfully submitted. Save this information for your future reference.
Timely Filling Limit
- Optum Care Claims: Submitting claims can be done in both ways electronically or on paper. But submission needs to be done before there are required time frames. Timely filing limit for Optum Care Claims is 90 days or per the provider contract. After 90 days claim submission will not be entertained.
- UnitedHealthcare (UHC): The timely filing limit for submitting claims to UnitedHealthcare (UHC) – 90 calendar days or based on the specific plan and contract between the healthcare provider and UnitedHealthcare. It’s essential for healthcare providers to be aware of the terms and conditions outlined in their provider contracts to avoid claim denials due to missed timely filing deadlines.
Phone Number for Claim Status – UnitedHealthcare Provider Portal
| EDI: Medical claims payer ID | 87726 |
| Dental claims payer ID | 95378 |
| Phone Number | 1-866-509-1593 |
How to claim in uhc (Umc) provider portal online?
- Apply online to claim status on online portal of UnitedHealthcare Provider Portal
- Visit official website of UnitedHealthcare Provider Portal – uhcprovider.com
- Now Sign In to UnitedHealthcare Provider Portal with your user ID and password
After sign in select Claims & Payments on homepage menu - Now fill details and upload documents asked in a claim form
- Submit the claim electronically and save it for future reference
Important Links
| UHC Claim Provider Portal | Click here |
| Optum Claim Provider Portal | Click here |
Further Asked Questions
Optum Provider Portal website – www.optum.com or
UMC stands for United Medical Center, while UHC likely stands for UnitedHealthcare. UHC (UMC) is one of the largest health insurance providers in the United States.
Apply online to claim status on the online portal of UnitedHealthcare Provider Portal – uhcprovider.com